Pressure ulcers, bedsores, and decubitus are synonymous terms used to describe a condition that is rapidly becoming a major health problem. Pressure ulcers are localized areas of dying cells occurring over bony prominences which are subjected to continuous pressure for prolonged periods of time. Continuous pressure for long periods, known as passive loading, occludes nutrition from reaching the cells and causes metabolic waste to accumulate in the effected area.
Following a complete spinal cord injury, pressure ulcers are one of the most common problems faced by the patient and rehabilitation team. Pressure ulcers pose a serious and constant medical problem which, if not closely monitored, can result in extended hospitalization.
Approximately 60% of complete cervical cord injuries and more than 50% of paraplegics (complete thoracic and lumbar cord injuries) will develop pressure ulcers (Paraplegia, 19 (1981), 234-247). In addition, 32 percent of patients are readmitted to the hospital for treatment of pressure ulcers within 24 months of discharge (Journal of Rehabilitation R&D, 20 (1983), 74-83).
Prevention of pressure ulcers requires knowledge of current management procedures and continuous application of these procedures throughout the life of the patient with spinal cord injury. To achieve this goal, several important steps have been taken by the health care community in recent years.
First, Decubitus, a compendium of prevention and treatment of pressure ulcers, was first published in 1988 because of the growing health care cost related to this problem. Dr. Roberta Abruzzese, editor of Decubitis, notes that $6.5 billion is spent annually for pressure ulcer care (Decibitis,l (February, 1988), 7).
Second, because of a growing severity of the problem and a lack of understanding that most pressure ulcers can be prevented, a group of concerned professionals formed the National Pressure Ulcer Advisory Panel (NPUAP) in 1988. In its commitment to the prevention of pressure ulcers, the NPUAP influences legislation related to the problem.
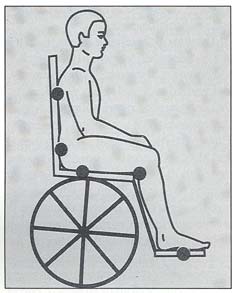
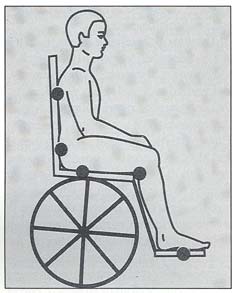
Most recently, in May of 1992, the Agency for Health Care Policy and Research (AHCPR), within the Department of Health and Human Services, developed national clinically relevant guidelines entitled,Pressure Ulcers in Adults: Prediction and Prevention. The purpose of the guidelines is to help define early interventions for prevention and management of Stage I (the least severe of the four stage condition) pressure ulcers. The guidelines suggest that risk to pressure ulcers decreases with skin inspection at least once a day, cleansing moist skin caused by urinary or fecal incontinence or perspiration, improvement in mobility and activity, and protection against the effects of external mechanical forces (e.g., pressure, friction, and shear).
Dr. Martin Ferguson-Pen, Director of the Center for Rehabilitation, West Haverstraw, New York, known for his bioengineering research related to pressure relief, has hypothesized that "pressure ulcers in athletes are not due to pressure loading but to active loading. Athletes, when competing, tend to create forces sufficiently high enough to cause localized tearing and shearing of tissue and blood vessels which can cause a pressure ulcer to develop."
Recently, attention has been given to the prevention and treatment of pressure ulcers among athletes with disabilities. National Handicapped Sports will disqualify any athlete with a pressure ulcer from seimming competition. In addition the "Code of Conduct" established by the U.S. Disabled Sports Team for the 1992 Paralympics held in Barcelona addressed pressure ulcers for the first time. Rule 25 states that "Athletes with open would requiring daily treatment will not be permitted to participate in competition."
Because of these developments, should the U.S. Olympic Committee study the prevalence and severity of pressure ulcers among athletes who vie for the U.S. Disabled Sports Team? Are studies needed to address product efficiency (e.g., cusions and wheelcahirs) related to pressure culcer reduction among athletes with disabilities?
Another concern is children with spinal cord injury. Dr. Nancy Bergstrm, Chairperson of the AHCPR panel, states that "most of the AHCPR guidelines are appropriate for children and youth but there is a dearth of research on pressure ulcers in younger genrations." Given the growing incidence of wheelchair users among children and youth, should specific pediatric pressure ulcer guidelines be developed? Another issue is that of awareness-- are teachers and ohter professionals in your schoos and community organizations aware of the potential severity of pressure ulcers? Finally, what steps can be taken to further heighten awareness of this condition and reduce the risk of hospitalization?